| To Register SMDM Homepage | |

|

|
|
||||
Purpose: In a trial comparing two radiotherapy schedules for palliation of non-small-cell lung cancer, the longer schedule unexpectedly provided significantly better survival. A model was constructed to estimate lifelong costs and quality adjusted life years.
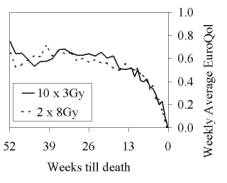 Methods: Patients were randomized to receive a 10 x 3Gy or a 2 x 8Gy radiotherapy schedule (n=297, median age 69 years, tumor stage IIIA/B or IV). They were followed for at most one year, with symptom palliation as primary outcome measure. Utility was measured using the EuroQol classification system. Societal costs were measured only during the initial 12 weeks, using questionnaires in a subset of 56 patients. There were three types of missing data: 10% of the patients were alive at study closure, about 20% of the questionnaires were not returned, and cost questionnaires were returned for at most 12 weeks. Neglecting missing data would lead to bias, because at the end of follow-up there were significant differences in survival (13% versus 7%, p=0.05) and utility (0.28 versus 0.17, p=0.03). The observed relationships between utility, remaining lifetime and costs were used to model censured survival times and missing utility and costs data.
Methods: Patients were randomized to receive a 10 x 3Gy or a 2 x 8Gy radiotherapy schedule (n=297, median age 69 years, tumor stage IIIA/B or IV). They were followed for at most one year, with symptom palliation as primary outcome measure. Utility was measured using the EuroQol classification system. Societal costs were measured only during the initial 12 weeks, using questionnaires in a subset of 56 patients. There were three types of missing data: 10% of the patients were alive at study closure, about 20% of the questionnaires were not returned, and cost questionnaires were returned for at most 12 weeks. Neglecting missing data would lead to bias, because at the end of follow-up there were significant differences in survival (13% versus 7%, p=0.05) and utility (0.28 versus 0.17, p=0.03). The observed relationships between utility, remaining lifetime and costs were used to model censured survival times and missing utility and costs data.
Results: For the 10 x 3Gy and 2 x 8Gy schedules respectively, average life expectancy was estimated at 35 and 26 weeks (p=0.02) and quality adjusted at 19 and 12 weeks (p=0.03). The differences were larger and more significant than for the non-extrapolated data. Radiotherapy costs were estimated at €3.700 and €2.200 (p<0.001) and non-radiotherapy costs at €5.900 and €5.000 (p=0.17), with estimated cost-utility ratio 19.000 €/QALY. Without taking costs during the additional lifetime into account, the cost-utility ratio would have been 12.000 €/QALY.
Conclusions: The increase in life expectancy (36%) for the longer radiotherapy schedule led to a less than proportional increase in non-radiotherapy costs (19%), because part of the costs were associated with the deteriorating health preceding death. Including the costs during the additional lifetime led to a higher but still acceptable cost-utility ratio.
See more of Oral Concurrent Session B - Health Economics
See more of The 26th Annual Meeting of the Society for Medical Decision Making (October 17-20, 2004)