Burhaneddin Sandikci, MS, University of Pittsburgh, Pittsburgh, PA, Oguzhan Alagoz, PhD, University of Wisconsin, Madison, WI, Lisa Maillart, PhD, Case Western Reserve University, Cleveland, OH, Andrew Schaefer, PhD, University of Pittsburgh, Pittsburgh, PA, and Mark S. Roberts, MD, MPP, University of Pittsburgh, Pittsburgh, PA.
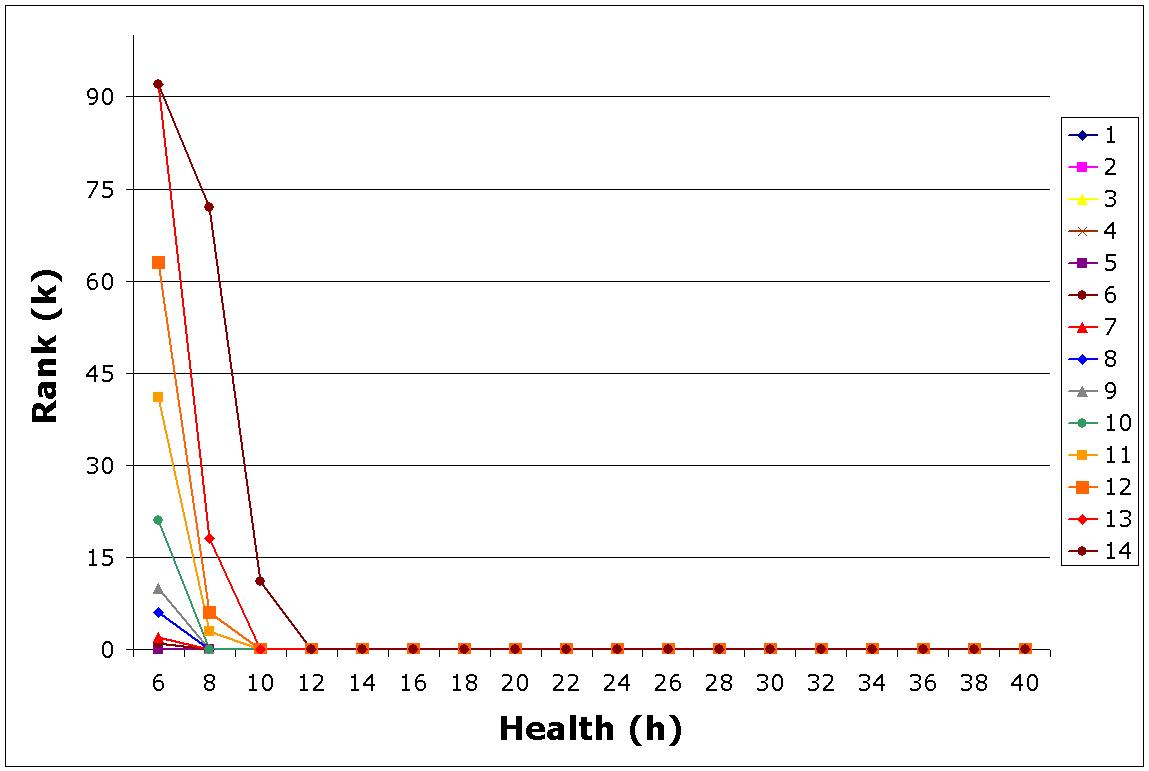
Purpose. Currently, patients waiting for a cadaveric liver have little information regarding their position on the waiting list. This study aims to evaluate whether knowledge of specific location on the waiting list changes the optimal accept/reject decision for a given donor organ and shows the value of making the waiting list information transparent. Methods. We model the problem of accepting or rejecting a liver offer as a Markov decision process (MDP). The state of the system is composed of the triplets (h,k,l), where ‘h' represents the health status of the patient, ‘k' is the rank of the patient in the waiting list for the current liver offer, and ‘l' is the quality of the liver as determined by the characteristics of the donor such as age, gender, race, etc. The transition probabilities of the system are estimated using the natural history of liver disease as well as a previously validated national liver allocation simulation model. Optimal accept/reject decisions are found using the policy iteration algorithm. Results. The optimal accept/reject decisions take a ‘control-limit' form as shown in the figure. The horizontal axis shows the health of the patient as measured by MELD score. (Higher MELD scores represent sicker patients). The possible ranks of the patient are displayed on the vertical axis, where a zero rank is interpreted as the patient being off of the waiting list at the current stage. Each line represents a different organ quality where organ quality decreases from 1 to 14. For each organ quality, the area is split into two regions by the threshold line, where the optimal action is to ‘reject' the offer below the line (inclusive) and to ‘accept' the offer above the line. For the first 5 organ qualities (i.e., the top five quality organs) the optimal action is always to ‘accept' regardless of the health/rank combination (i.e., the lines associated for these organs coincide with the horizontal axis). If the organ quality further decreases, the rank threshold increases. In general, the reject region becomes larger as the quality of the organ decreases. Conclusion. The probabilistic model used shows that the optimal decision changes significantly if the waiting list information is known to the decision maker (patient/surgeon).
See more of Poster Session III
See more of The 28th Annual Meeting of the Society for Medical Decision Making (October 15-18, 2006)

