|
||||
Tuesday, October 23, 2007
P3-16
A DOUBLE CHAIN APPROACH TO ESTIMATION OF VISION RELATED UTILITIES
Methods: Between June 1998 and October 1999 443 patients from 18 ophthalmic practices were interviewed using the standard gamble): diabetic retinopathy (DR) =59, glaucoma=99, and macular degeneration (AMD)=44. Participants were asked to respond to four scenarios: the vision scale (perfect vision---current vision---unilateral blindness: scenario P1), the comorbidity scale (perfect health---current health---death, with instruction to assume the participant currently has perfect vision: scenario P2), and a scenario for unilateral blindness (perfect vision---unilateral blindness---death: scenario P3), and the policy scale (perfect health---current health---death: scenario PS). Vision specific on the policy scale was estimated by the chain: (P1 * P2) + [(1-P1) * P3]. Vision specific disutility is given by subtracting P2 from the result of this equation.
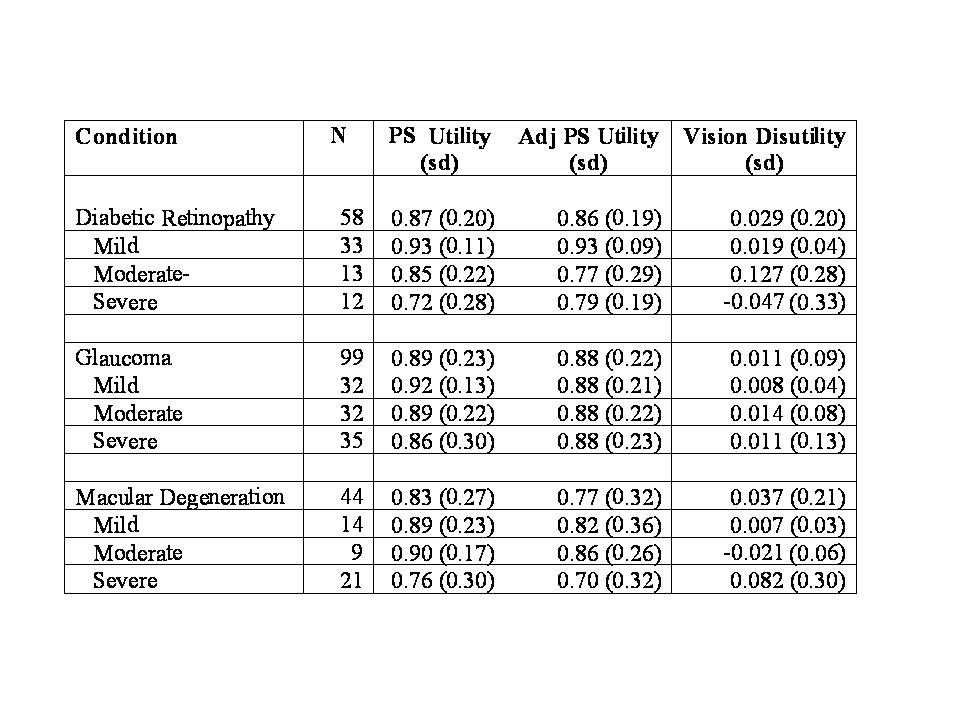
Results: The results are provided in the attached table. The ordering of overall utility loss (macular degeneration most utility loss, glaucoma least) has face validity, but is considerably less than that reported by previous investigators conducting utility elicitation in people with chronic vision problems on the vision-truncated policy scale (i.e., perfect vision---current vision---death), a non-standard method of elicitation, but widely used in ophthalmology. Within each disease the general trend across severity reflects the expected pattern, as seen in the PS scenario, except where cell sizes are particularly small (i.e., severe diabetic retinopathy and moderate AMD). However, again, the pattern reflects lower utility loss than previously reported.
Conclusions: Additional investigation is needed in larger samples, but the proposed double chain method has promise as a future method to elicit utilities related to vision. However, if the level of reported utility loss is borne out, it may indicate problematic aspects related to current estimates of utility loss in vision.