|
||||
Monday, October 22, 2007 - 4:15 PM
C-2
ESTIMATING THE PATIENT'S PRICE OF PIRVACY IN LIVER TRANSPLANTATION
Methods. The organ accept/reject decision is modeled as a Markov decision process. The state of the process is the current patient health, quality of the offered liver, and the rank of the patient on the WL. Patient health is described by the MELD score (the sicker the patient the higher her MELD score); and the liver quality is described by a combination of characteristics of the donor and the recipient. Transition probabilities of the process are estimated using the natural history of liver disease as well as a validated national liver allocation simulation model. The objective of the decision process for each patient is to maximize the total expected pre- and post-transplant life. To quantify patient benefit, a patient's price of privacy (pPoP) is defined as the percentage of expected life days gained due to more transparent WL information. The implicit waiting list model of Alagoz et al. (2007) is used to obtain pPoP estimates for 200 sample patients with various diseases. The model is calibrated with data from UNOS and a large urban transplant hospital. The optimal decision rules are found using the policy iteration algorithm.
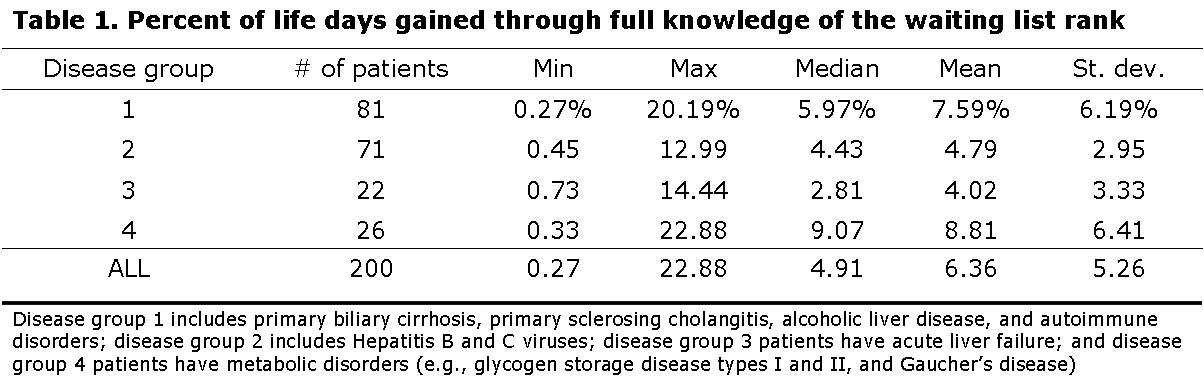
Results. Overall, patients could increase their total survival by an average of 6% by incorporating knowledge of their position on the WL in their decision, although the benefit varied by disease: acute patients gained the least at only 4.02% (Table 1). The distribution of potential benefits across patients is large: some patients gained less than 0.5% of their survival time, while others gained over 20%.
Conclusions. The probabilistic model analyzed shows that the optimal decisions change significantly if the waiting list information is known to the decision maker (patient/surgeon). A patient's price of privacy is estimated to be on the order of 5% of her maximum survival achieved without WL information.