|
||||
Wednesday, October 24, 2007 - 11:30 AM
I-5
WHEN TO START ANTIRETROVIRAL THERAPY AND PREVENTIVE TREATMENT FOR LATENT TUBERCULOSIS INFECTION FOR HIV-INFECTED PATIENTS IN RESOURCE-LIMITED SETTINGS
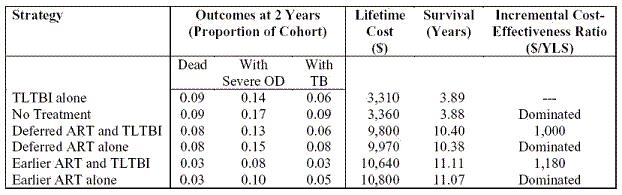
Purpose: Debate over when to initiate antiretroviral therapy (ART) for HIV has led to the design of several “when to start” trials comparing “earlier ART” (CD4 <350/µl) to current World Health Organization recommendations (before CD4 < 200/µl). Our objective was to examine strategies for ART initiation in South Africa, with and without preventive treatment for latent TB infection (TLTBI). Methods: We used a state-transition model of HIV disease (CEPAC-International) to simulate different treatment strategies. For a cohort with mean CD4 count 375/µl (SD 10/µl) and mean age 32.8 years, we projected life expectancy (LE), costs, and cost-effectiveness for 6 strategies: 1) no treatment (natural history); 2) TLTBI alone (9-month course initiated immediately); 3) “deferred” ART alone (initiated at CD4 <250/µl or severe opportunistic disease [OD]); 4) deferred ART and TLTBI; 5) “earlier” ART alone (initiated at CD4 <350/µl) and 6) earlier ART and TLTBI. Natural history and healthcare utilization data were from the Cape Town AIDS Cohort study. The base case assumed two sequential ART regimens with 48-week viral suppression of 73% and 58% obtained from published literature. TLTBI was assumed to be effective in preventing reactivation (28% of active TB cases in South Africa), but had no effect on TB reinfections and subsequent progression to active disease. Sensitivity analyses varied incidence of TB reactivation and reinfection, TLTBI and ART efficacy, ART switching and stopping criteria, and costs. Results: All ART strategies increased mean LE by over 6.5 years compared to those without ART. Earlier ART reduced severe ODs and deaths in the first 2 years. Strategies incorporating TLTBI were cost-saving compared to those without, but LE gains from TLTBI were less than 0.1 year. Although mean survival was sensitive to efficacy of first-line ART and ART switching and stopping criteria, varying these parameters had little impact on incremental cost-effectiveness ratios. Conclusions: Earlier initiation of ART in HIV-infected patients in South Africa improves short- and long-term survival and is cost-effective. While awaiting results of prospective trials, this analysis suggests earlier initiation of ART with TLTBI should be the treatment goal in South Africa.