|
||||
Monday, October 22, 2007 - 4:30 PM
D-3
CAN VIDEO DECISION AIDS IMPROVE THE MATCH BETWEEN PATIENTS' PREFERENCES AND CHOICES?
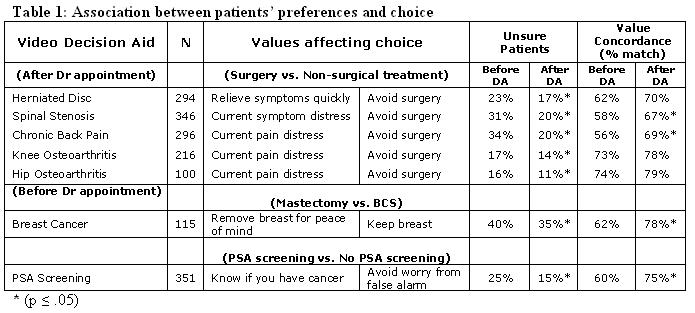
Methods: Eligible patients were systematically referred to the Center for Shared Decision Making at Dartmouth Hitchcock Medical Center. Participants: 1) complete pre-DA questionnaire, 2) watch a condition specific video decision aid, 3) complete post-DA questionnaire. Measures: pre/post-video intention, values (category scale: 1-10 importance). DA topics included: herniated disc, spinal stenosis, chronic back pain, knee and hip osteoarthritis, breast cancer surgery, and PSA screening.
The following methodology was developed to calculate value concordance (% match): 1) Use multivariate logistic regression to test value scores as predictors of choice, 2) Run a 10-fold cross-validation to fit the logistic regression model and calculate the predicted probability of choice for each observation, and 3) Test how well the validation model predicts patient choice (e.g., before video vs. after video).
Results: Across a diverse array of conditions, similar patterns emerged (Table 1). After watching the video decision aid: 1) a pair of contrasting values was selected by each logistic model, 2) fewer patients were unsure (χ2, p ≤ .05), and 3) more patients chose the option predicted by their value scores.
Conclusions: Using a logistic-regression approach, we were able identify key predictors associated with specific medical decisions. The value concordance (% match) is the proportion of patients whose preference scores accurately predict their intended choice. For these patients, video decision aids improved the match between their preferences and intended choice.